Skin Problems Associated with Menopause and Birth Control Pills.
Skin Problems Associated with Menopause and Birth Control Pills.
Menopause
Menopause is the time in a woman’s life when the ovaries stop releasing ova.
It is normally occurs when a woman is in her late forties or early fifties.
The time before and around menopause is called perimenopause.
What happens during menopause is that the ovaries have run out of follicles containing eggs.
A female is born with 700,000 to 2 million eggs, which are contained in the follicles within the ovaries.
Many of these eggs soon die or atrophy, but at puberty about 400,000 remain.
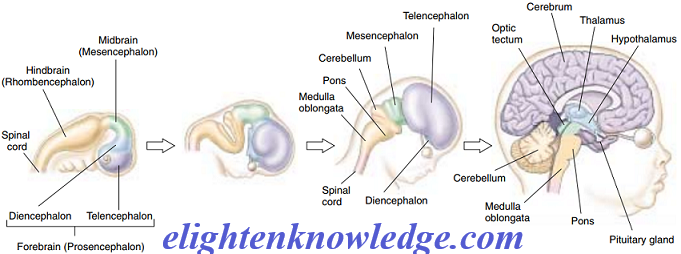
The pituitary gland secretes FSH and LH, but the ovaries stop responding.
When no follicles are left to respond to follicle-stimulating hormone, no oestrogen is produced in the ovary, and the preparation of the uterus does not occur.
You may also want to read;
- The Adrenal Gland and Stress Responses
- Understanding the Hormonal Control of the Male and Female Reproductive System.
- Production Gametes (Sperm cell and Eggs/Oocytes)
- Why you feel pains in the muscle after strenuous exercise?
The drop in hormone levels in the bloodstream causes a variety of physical symptoms;
- Hot flashes,
- rapid heartbeat,
- decrease in vaginal secretions,
- emotional irritability,
- bloating,
- and other signs may occur.
The same symptoms may be produced after a hysterectomy.
If a woman has a hysterectomy early in life, the gynaecologist often leaves the ovaries and removes only the uterus.
The presence of the ovaries helps secure hormone levels in the bloodstream, at least until true menopause takes place.
Medical science has discovered that women who lose their ovaries early in life are more likely to develop osteoporosis, a weakening of the bones that is associated with aging and is predominant in women.
Many women have hormone replacement therapy (HRT) after menopause or after a hysterectomy.
The use of synthetic oestrogen and progesterone, taken in the sequence of the normal menstrual cycle hormone secretions, helps prevent many of the symptoms associated with menopause.
It, of course, does not make women ovulate again.
Oestrogen is believed to have a positive effect on reducing the chances of osteoporosis development, offers a decreased chance of cardiac problems, and may help prevent rheumatoid arthritis.
Some recent studies indicate that the risk of breast cancer may increase in women who use HRT longer than five years.
If there is a history of breast cancer in the immediate family (sister, mother), there may be a greater risk.
The use of HRT should be an individual and personal decision based on personal and family history; menopausal symptoms and their severity; and, most importantly, a thorough consultation with a doctor.
SKIN CONDITIONS ASSOCIATED WITH MENOPAUSE
In the next two decades, 40 million women will go through menopause.
A Woman may have any number of symptoms associated with perimenopause.
This may include;
- thinning hair,
- excess hair growth on the face or other body areas,
- or even increased oiliness or dryness of the skin.
Today an abundance of research indicates that the presence of oestrogen strongly influences collagen formation.
As menopause occurs, oestrogen levels drop dramatically and may have an obvious effect on the appearance of wrinkles and lack of elasticity.
Use of HRT may improve and reduce the loss of collagen, therefore causing the skin to regain more of its previous elasticity and suppleness.
Lack of oestrogen may significantly affect
- barrier function,
- increasing sensitivity of the skin,
- dehydration,
- possible hyperpigmentation,
- and fluctuations in blood flow.
Oestrogen is responsible for sending many hormonal messages to the skin, and a decrease can affect many functions of the skin and, therefore, its appearance.
Many aging problems associated with menopause may be the result of cumulative sun exposure earlier in life.
Coincidentally, the damage from years of sun exposure happens to surface at about the same time as menopause in some women.
Having both sun damage and menopausal effects on the skin can cause real aesthetic problems and is even more reason that it needs lots of care at this important time.
Hot Flashes and Flushing
- Hot flashes are caused by a fluctuation in blood fl ow resulting from decreased oestrogen, which normally helps with smooth blood fl ow.
- Without oestrogen, there are sudden “spurts” in blood flow, resulting in redness and the feeling of heat in the skin.
- Flushing and hot fl ashes can be reduced or eliminated with hormone replacement therapy.
- Rarely, do women experience a condition called formication, which feels like continuous tingling and itching.
- Some women have described it as feeling like “bugs crawling on the skin.”
- Again, this condition can be treated with HRT.
- The use of fragrance-free creams with lipid replacement ingredients such as sphingolipids or ceramides may help with dryness and itching.
- The skin may be more sensitive to any stimulating product, so be careful with these, especially the stimulating aromatherapy products.
Moodiness
- Women may experience moodiness during menopause.
- Although some of this may be caused by hormonal fluctuations, it may also be stress-related or may be complicated by depression.
- It is important to be understanding of the needs of your client who is menopausal and to offer stress-reducing services such as massages or aromatherapy.
Perimenopausal Acne
- Some women may experience a sudden flare-up of acne during or just after menopause.
- This is again caused by a decrease of oestrogen in the bloodstream, which in turn increases the percentage of the male hormone androgen that turns on the sebaceous glands.
- This results in increased oiliness, hirsutism, and acne lesions.
- You should treat this as you would any other acne case, but remember that the client may more readily experience dehydration and be concerned about aging skin.
- Be careful not to over-dry the skin.
Aesthetic Management of Menopausal Skin
- The aesthetician can play a significant role in helping the women going through menopause with skin problems.
- The aesthetician may notice small symptoms in the skin before the client is even fully aware that she is beginning menopause.
- Keep the person’s age in mind when noticing some of the symptoms we have discussed here.
- Adjusting the person’s home care and treatment schedule may greatly help.
Menopausal Skin Symptoms
- Dryness and itchy skin on the face and body
- Increased sensitivity
- Sudden flares of acne
- Sudden hair growth on the face
- Mood swings
- “Suddenly aging” skin
- Hot fl ashes and fl ushing
- A “tired” look to the skin, with increased elastosis
A Treatment Plan for the Menopausal Skin
Although symptoms can vary from dryness to acne, the following guidelines should help with most of the age-related symptoms of menopause.
- Daily use of sunscreen/moisturizer. Make sure the moisture base is appropriate for the skin type. Make sure the sunscreen is broad spectrum and has a sun protection factor (SPF) of 15 or higher.
- Use of alpha hydroxy acids daily helps improve the appearance of wrinkles and hyperpigmented splotching, increases moisture in both the epidermis and the dermis, improves cell turnover that improves barrier function, less skin flakiness, and improves surface texture and feel of the skin. Make sure you use a product appropriate for the skin type. Usually, the best choice for this time of life is a serum applied under a moisturizer.
- Retinoids such as retinol are vitamin A-based ingredients that also can help reduce the appearance of sun damage. Retinol should be used carefully since it sometimes produces irritation.
- Use of topical antioxidants helps prevent reactions that lead to further collagen breakdown; their use also may help prevent inflammation and redness.
- Use of topical phytoestrogens, which are plant hormones frequently seen in ingredients like soy sterols, wild yam extract, and red clover extract.
- For dry skin, home-care moisturizers or body lotions containing lipid ingredients such as ceramides or sphingolipids help reinfuse the barrier function with lipids, improve dryness, diminish wrinkles, increase firmness, and make the skin feel better and less itchy.
- Facial creams or serums that contain peptides and collagen stimulants will help the skin look firmer and more supple as well as decrease the appearance of elastosis and wrinkling.
Here are some salon treatments advised for the menopausal conditions:
- Alpha hydroxy exfoliation (peels), beginning with a series and then maintaining the results with follow-up alpha-hydroxy treatments. These exfoliation treatments, along with the alpha hydroxy home care recommended above, often make a big difference in the skin’s appearance relatively quickly.
- Microcurrent treatments, again administered in a series of treatments, improve elasticity and help stimulate the skin to look healthier.
- Light-emitting diode (LED) treatments use rapidly flashing light energy to stimulate the skin, resulting in a younger-looking appearance and less redness.
- More frequent salon treatments, including facial and body massage, may help with aesthetic symptoms as well as help the individual with stress management.
Lastly, clients experiencing menopausal symptoms should always consult with a board-certified gynaecologist or endocrinologist.
Diet changes and stress-reducing programs often can help with the many symptoms of menopause.
BIRTH CONTROL PILLS
Birth control pills work by regulating hormones normally associated with the menstrual cycle.
They interfere with the normal development of the ovum by preventing or obstructing ovulation.
There are two basic types of birth control pills.
One type contains both oestrogen and progesterone and works by preventing the egg from maturing, therefore preventing ovulation.
The other type is mainly progesterone.
These are often called mini-pills.
They work by exposing the bloodstream to extra amounts of progesterone, which causes thickening of the uterine fluids and thus keeps the egg from becoming fertile.
Skin Problems Associated with Birth Control Pills
- A skin problem often associated with the use of birth control pills is the tendency to have acne flare-ups.
- This does not occur in all women using birth control pills, but it does occur in a substantial number.
- Aestheticians commonly see acne flares in patients who have just started using a new type of birth control pill.
- The hormones in the pills change normal hormone levels, affecting sebum production.
- Birth control pills that contain little or no oestrogen tend to be more aggravating to acne conditions.
- Oestrogen-dominant pills tend to improve acne-prone skin.
In the past,
- Birth control pills with high levels of hormones often caused very frequent acne flares.
- More modern birth control pills contain smaller amounts of hormones and do not cause as many problems with acne flares.
Starting and stopping birth control pills may dramatically affect acne.
- Starting an androgen-dominant or progesterone-dominant pill may make acne immediately worse, whereas starting an oestrogen-dominant pill may make acne-prone skin immediately better.
- Stopping the pill may have similar effects.
- Because the pill tends to suppress natural hormone levels, discontinuing the pill may throw off natural hormone levels, making acne worse.
- It may take some time for the body to adjust to not having the hormone “supplement” present in the birth control pills.
- Some women take much longer to adjust.
Hyperpigmentation and the Birth Control Pill
- The other appearance problem related to birth control pills is that of hyperpigmentation or melasma.
- Splotchy, pigmented complexions may be present after the use of birth control pills.
- This hyperpigmentation usually is located in the forehead and cheeks.
- The upper lip is also often affected by melasma.
- Some women can develop a full-scale pregnancy mask associated with birth control pills.
- Sunlight, especially deliberate exposure such as sunbathing, can make melasma much worse.
- Advise a client with melasma to stay out of the sun.
- If she must go in the sun, recommend the use of a high-SPF, broad-spectrum sunscreen.
- Sometimes the doctor can adjust the dosage or the type of the pill to reduce the possibility of melasma resulting from its use.
- You should treat hyperpigmentation with hydroquinone and glycolic acid.
- Prescription topical drugs specifically designed to treat melasma are also available.
- One of these is Triluma, which is a topical combination of hydroquinone, tretinoin (the active ingredient in Retin-A®), and a steroid.
- This combination has proven effective in many cases of melasma.
Join Enlighten Knowledge WhatsApp platform.
Join Enlighten Knowledge Telegram platform.