How to Detect Kidney Failure, Causes, And Effects
How to Detect Kidney Failure, Causes, And Effects
Content:
- Causes and effects of kidney failure
- Measuring glomerular filtration rate (GFR)
- Treating kidney failure with dialysis
- Haemodialysis
- Peritoneal dialysis.
- Treating kidney failure by transplant
- Dialysis or transplant?
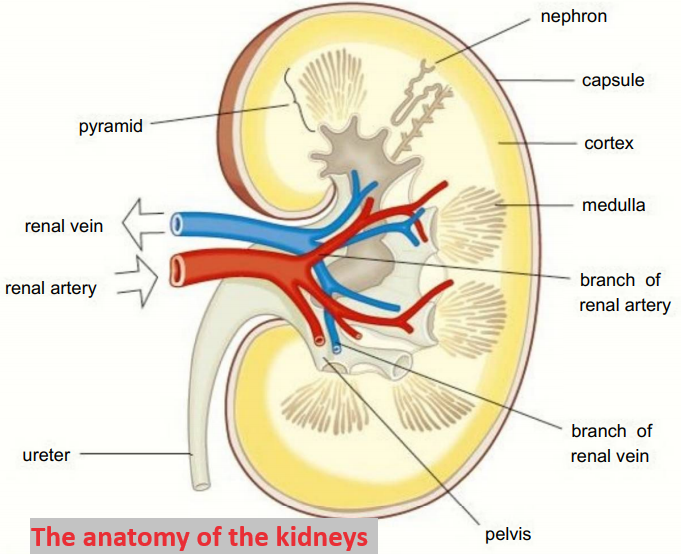
The kidneys play a vital role in homeostasis.
If they are damaged and become less efficient or stop working, the effects on the body are serious and may be fatal if they are not treated.
Causes and effects of kidney failure
There are a number of reasons why the kidneys may fail.
They include;
- Kidney infections, where the structure of the podocytes and the tubules themselves may be damaged or destroyed.
- Raised blood pressure that can damage the structure of the epithelial cells and basement membrane of the Bowman’s capsule.
- And genetic conditions such as polycystic kidney disease where the healthy kidney tissue is replaced by fluid-filled cysts or damaged by pressure from cysts.
If the kidneys are infected or affected by high blood pressure, this may cause:
- Protein in the urine. If the basement membrane or podocytes of the Bowman’s capsule are damaged, they no longer act as filters and large plasma proteins can pass into the filtrate and are passed out in the urine.
- Blood in the urine. Another symptom that the filtering process is no longer working.
If the kidneys fail completely, the concentrations of urea and mineral ions build up in the body. The effects include:
-
Loss of electrolyte balance
When the kidneys fail, the body cannot excrete excess sodium, potassium, and chloride ions. This causes osmotic imbalances in the tissues and eventual death.
-
Build-up of toxic urea in the blood
If the kidneys fail, the body cannot get rid of urea and it can poison the cells.
-
High blood pressure
The kidneys play an important role in controlling the blood pressure by maintaining the water balance of the blood. If the kidneys fail, the blood pressure increases and this can cause a range of health problems including heart problems and strokes.
- Weakened bones as the calcium/phosphorus balance in the blood is lost.
- Pain and stiffness in joints as abnormal proteins build up in the blood.
- Anaemia
The kidneys are involved in the production of a hormone called erythropoietin that stimulates the formation of red blood cells. When the kidneys fail it can reduce the production of red blood cells causing tiredness and lethargy.
Measuring glomerular filtration rate (GFR)
Kidney problems almost always affect the rate at which blood is filtered in the Bowman’s capsules of the nephrons.
The glomerular filtration rate (GFR) is widely used as a measure to indicate kidney disease.
The rate of filtration is not measured directly – a simple blood test measures the level of creatinine in the blood.
Creatinine is a breakdown product of muscles and it is used to give an estimated glomerular filtration rate (eGFR).
The units are cnP/min.
If the levels of creatinine in the blood go up, it is a signal that the kidneys are not working properly.
Certain factors need to be taken into account in the calculations to work out GFR.
For example, GFR decreases steadily with age even if you are healthy, and men usually have more muscle mass and therefore more creatinine than women.
There are two main ways in which kidney failure is treated.
- In renal/kidney dialysis, the function of the kidneys is carried out artificially.
- In a transplant, a new healthy kidney is put into the body to replace the functions of the failed kidneys an animal can function perfectly well with just one healthy kidney.
Treating kidney failure with dialysis
Normal GFRs do not fall below 70 even in very elderly people.
A GFR of below 60 for more than three months is taken to indicate moderate to severe chronic kidney disease and if it falls below 15, that is kidney failure.
The kidneys are filtering so little blood meaning they are virtually ineffective.
There are two main types of dialysis;
- haemodialysis
- and peritoneal dialysis.
Haemodialysis
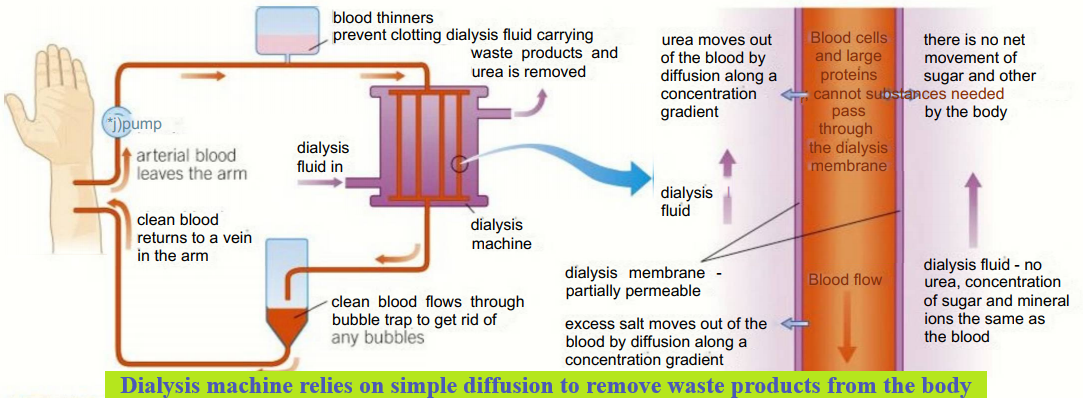
This involves the use of a dialysis machine.
It is usually carried out in hospital although sometimes patients will have a machine in their own home.
Blood leaves the patient’s body from an artery and flows into the dialysis machine, where it flows between partially permeable dialysis membranes.
These membranes mimic the basement membrane of the Bowman’s capsule.
On the other side of the membranes is the dialysis fluid.
During dialysis, it is vital that patients lose the excess urea and mineral ions that have built up in the blood.
It is equally important that they do not lose useful substances such as glucose and some mineral ions.
The loss of these substances is prevented by careful control of the dialysis fluid.
It contains normal plasma levels of glucose to ensure there is no net movement of glucose out of the blood.
The dialysis fluid also contains normal plasma levels of mineral ions, so any excess mineral ions in the blood move out by diffusion down a concentration gradient into the dialysis fluid, thus restoring the correct electrolyte balance of the blood.
The dialysis fluid contains no urea meaning there is a very steep concentration gradient from the blood to the fluid, and as a result, much of the urea leaves the blood.
The blood and the dialysis fluid flow in opposite directions to maintain a counter current exchange system and maximize the exchange that lakes place.
The whole process of dialysis depends on diffusion down concentration gradients, there is no active transport.
Dialysis takes about eight hours and has to be repeated regularly.
- Patients with kidney failure who rely on haemodialysis have to remain attached to a dialysis machine several times a week for many hours.
- They also need to manage their diets carefully, eating relatively little protein and salt and monitoring their fluid intake to keep their blood chemistry as stable as possible.
- The only time they can eat and drink what they like is at the beginning of the dialysis process.
-
Peritoneal dialysis
Peritoneal dialysis is done inside the body.
It makes use of the natural dialysis membranes formed by the lining of the abdomen, that is, the peritoneum.
It is usually done at home and the patient can carry on with their normal life while it takes place.
The dialysis fluid is introduced into the abdomen using a catheter.
It is left for several hours for dialysis to take place across the peritoneal membranes, so that urea and excess mineral ions pass out of the blood capillaries, into the tissue fluid, and out across the peritoneal membrane into the dialysis fluid.
The fluid is then drained off and discarded, leaving the blood balanced again and the urea and excess minerals removed.
Treating kidney failure by transplant
Long-term dialysis has some serious side effects.
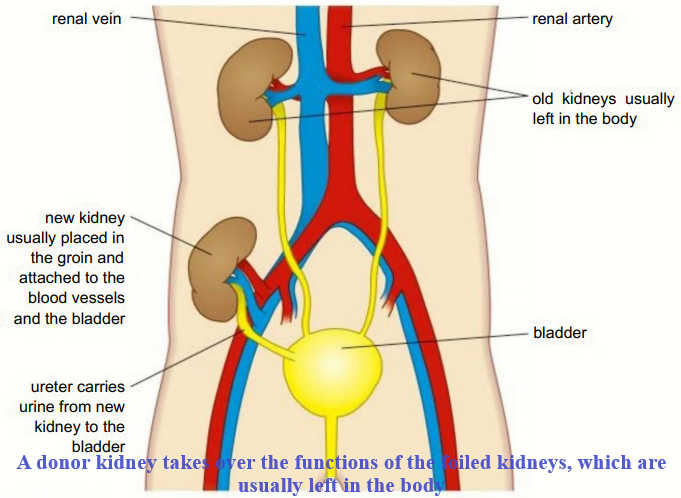
The best solution for the patient is a kidney transplant, where a single healthy kidney from a donor is placed within the body.
The blood vessels are joined and the ureter of the new kidney is inserted into the bladder.
If the transplant is successful the kidney will function normally for many years.
The main problem with transplanted organs is the risk of rejection.
- The antigens on the donor organ differ from the antigens on the cells of the recipient and the immune system is likely to recognise this.
- This can result in rejection and the destruction of the new kidney.
- There are a number of ways of reducing the risk of rejection.
- The match between the antigens of the donor and the recipient is made as close as possible.
- For example, a donor kidney can be used with a ’tissue type’ very similar to the recipient (from people with the same blood group).
- The recipient is given drugs to suppress their immune response (immunosuppressant drugs) for the rest of their lives.
- This helps to prevent the rejection of their new organ. Immunosuppressant drugs are improving all the time and the need for a really close tissue match is becoming less important.
- The disadvantage of taking immunosuppressant drugs is that they prevent the patients from responding effectively to infectious diseases.
- They have to take great care it they become ill in any way.
- However, most people feel this is a small price to pay for a new, functioning kidney.
- Transplanted organs don’t last forever with the average transplanted kidney functioning for around 9-10 years, although some have continued working for around 50 years.
Once the organ starts to fail the patient has to return to dialysis and wait until another suitable kidney is found.
Dialysis or transplant?
- Dialysis is much more readily available than donor organs, so it is there whenever kidneys fail.
- It enables the patient to lead a relatively normal life.
- However, patients have to monitor their diet carefully and need regular sessions on the machine.
- Long-term dialysis is much more expensive than a transplant and can eventually cause damage to the body.
- If a patient receives a kidney transplant, they are free from the restrictions which come with regular dialysis sessions and dietary monitoring.
- This is generally the ideal scenario for patients waiting for a transplant.
- The main source of donor kidneys is from people who die suddenly, often from road accidents, strokes, and heart attacks.
- In the UK, organs can be taken from people if they carry an organ donor card or are on the online donor register.
- Alternatively, a relative of someone who has died suddenly can give his or her consent.
Unfortunately;
- For people needing a transplant, there is a shortage of donor kidneys.
- Many people do not register as donors.
- In addition, as cars become safer, fewer people die suddenly in traffic accidents.
- Whilst good, this means there are fewer potential donors.
- At any one time there are thousands of people undergoing kidney dialysis.
- Most will not have the opportunity to have a kidney transplant.
- In 2011, scientists grew functioning embryonic kidney tissue from stem cells.
Going forward, the hope is that whole new kidneys can be grown perhaps even without the antigens which trigger the immune reaction so that patients don’t need to take immunosuppressant drugs.
Join Enlighten Knowledge WhatsApp platform.
Join Enlighten Knowledge Telegram platform.