Concise Biology Note on Blood vessels, Blood, Tissue Fluid, and Lymph
Content:
Introduction
The Blood Vessel
- Arteries and arterioles
- Capillaries
- Ways in which capillaries are adapted for their role
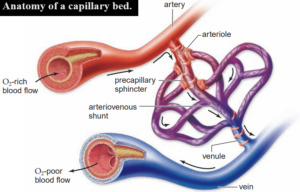
- Structure of the Capillary bed
- Veins and venules
Blood
- How deoxygenated blood return to the heart
- Functions of the blood
Tissue fluid
Lymph
Introduction:
It is estimated that if all the blood vessels of an average adult human were laid end to end, they would stretch to 100000 miles that is the equivalent of about four times around the circumference of the Earth.
There are several different types of blood vessels in the body and their structural composition is closely related to their function.
Some examples of different components utilised in some blood vessels are:
- Elastic fibres – these are composed of elastin and can stretch and recoil, providing vessel walls with flexibility.
- Smooth muscle – contracts or relaxes, which changes the size of the lumen (the channel within the blood vessel).
- Collagen – provides structural support to maintain the shape and volume of the vessel.
Arteries and arterioles
The arteries carry blood away from the heart to the tissues of the body.
They carry oxygenated blood except in the pulmonary artery, which carries deoxygenated blood from the heart to the lungs, and (during pregnancy) the umbilical artery, which carries deoxygenated blood from the foetus to the placenta.
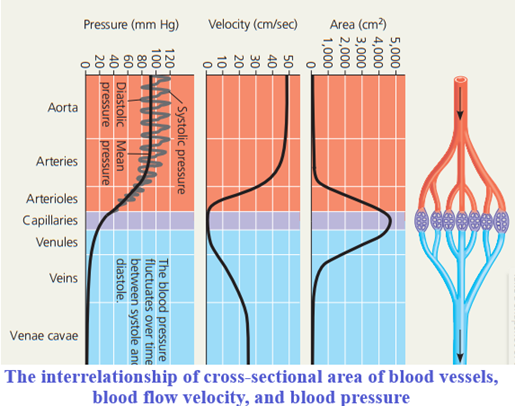
The blood in the arteries is under higher pressure than the blood in the veins.
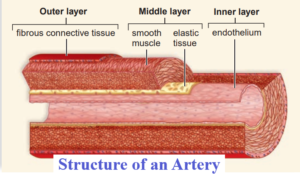
Artery walls contain elastic fibres, smooth muscle and collagen.
The elastic fibres enable them to withstand the force of the blood pumped out of the heart and stretch (within limits maintained by collagen) to take the larger blood volume.
In between the contractions of the heart, the elastic fibres recoil and return to their original length.
This helps to even out the surges of blood pumped from the heart to give a continuous flow.
However, you can still feel a pulse (surge of blood) when the heart contracts, which the elastic fibres cannot completely eliminate.
The lining of an artery’ (endothelium) is smooth so the blood flows easily over it.
Arterioles
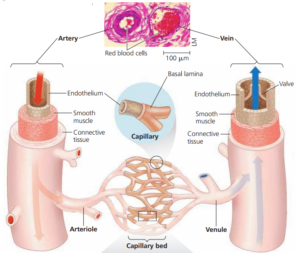
Arterioles link the arteries and the capillaries.
They have more smooth muscle and less elastin in their walls than arteries, as they have little pulse surge, but can constrict or dilate to control the flow of blood into individual organs.
When the smooth muscle in the arteriole contracts it constricts the vessel and prevents blood flowing into a capillary bed.
This is vasoconstriction.
When the smooth muscle in the wall of an arteriole relaxes, blood flows through into the capillary bed.
This is vasodilation.
Capillaries
The capillaries are microscopic blood vessels that link the arterioles with the venules.
They form an extensive network through all the tissues of the body.
The lumen of a capillary is so small that red blood cells (which have a diameter of only 7.5-8 pm) have to travel through in single file.
Substances are exchanged through the capillary walls between the tissue cells and the blood.
The gaps between the endothelial cells that make up the capillary walls in most areas of the body are relatively large.
This is where many substances pass out of the capillaries into the fluid surrounding the cells.
The exception is the capillaries in the central nervous system, which have very tight junctions between the cells.
In most organs of the body the blood entering the capillaries from the arterioles is oxygenated.
By the time it leaves the capillaries for the venules it has less oxygen and more carbon dioxide (it is deoxygenated).
Again, the lungs and the placenta arc the exceptions, with deoxygenated blood entering the capillaries and oxygenated blood leaving in the venules.
Ways in which capillaries are adapted for their role:
- They provide a very large surface area for the diffusion of substances into and out of the blood.
- The total cross-sectional area of the capillaries is always greater than the arteriole supplying them so the rate of blood flow falls.
- The relatively slow movement of blood through capillaries gives more time for the exchange of materials by diffusion between the blood and the cells.
- The walls are a single endothelial cell thick, giving a very thin layer for diffusion.
Structure of the Capillary bed:
When a capillary bed is open, sphincter muscles are relaxed and blood flows through the capillaries.
When precapillary sphincter muscles are contracted, the bed is closed and blood flows through an arteriovenous shunt that carries blood directly from an arteriole to a venule.
Veins and venules
The veins carry blood away from the cells of the body towards the heart and, with two exceptions, they carry deoxygenated blood.
The pulmonary vein carries oxygenated blood from the lungs to the heart, and (during pregnancy) the umbilical vein carries oxygenated blood from the placenta to the foetus.
Deoxygenated blood flows from the capillaries into very small veins celled venules and then into larger veins.
Finally, it reaches the two main vessels carrying deoxygenated blood back to the heart.
- The inferior vena cava from the lower parts of the body
- And the superior vena cava from the head and upper body.
Veins do not have a pulse thus, the surges from the heart pumping are lost as the blood passes through the narrow capillaries.
However, they do hold a large reservoir of blood up to 60% of your blood volume is in your veins at any one time.
The blood pressure in the veins is very low compared with the pressure in the arteries.
Medium-sized veins (the majority of the venous system) have valves to prevent the backflow of blood (see next page).
The walls contain lots of collagen and relatively little elastic fibre, and the vessels have a wide lumen and a smooth, thin lining (known as the endothelium) so the blood flows easily.
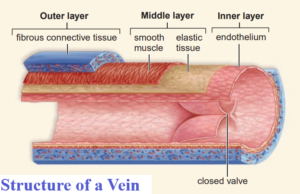
Venules
Venules link the capillaries with the veins.
They have very thin walls with just a little smooth muscle.
Several venules join to form a vein.
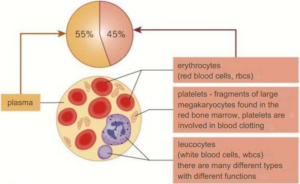
Blood
Blood consists of a yellow liquid – plasma – which carries a wide variety of other components including dissolved glucose and amino acids, mineral ions, hormones, and the large plasma proteins including albumin (important for maintaining the osmotic potential of the blood), fibrinogen (important in blood clotting) and globulins (involved in transport and the immune system).
Plasma also transports red blood cells (which carry oxygen to the cells and also give the blood its red appearance) and the many different types of white blood cells.
It also carries platelets.
Platelets are fragments of large cells called megakaryocytes found in the red bone marrow, and they are involved in the clotting mechanism of the blood.
Plasma makes up 55% of the blood by volume and much of that volume is water.
Only the plasma and the red blood cells are involved in the transport functions of the blood.
The other components have different functions.
How deoxygenated blood return to the heart
Deoxygenated blood in the veins must be returned to the heart to be pumped to the lungs and oxygenated again.
However, the blood is under low pressure and needs to move against gravity.
There are three main adaptations that enable the body to overcome this problem:
- The majority of the veins have one-way valves al intervals. These are flaps or infoldings of the inner lining of the vein. When blood flows in the direction of the heart, the valves open so the blood can pass through. If the blood starts to flow backwards, the valves close to prevent this from happening.
- Many of the bigger veins run between the big, active muscles in the body, for example in the arms and legs. When the muscles contract they squeeze the veins, forcing the blood towards the heart. The valves prevent backflow when the muscles relax.
- The breathing movements of the chest act as a pump. The pressure changes and the squeezing actions move blood in the veins of the chest and abdomen towards the heart.
Functions of the blood
The composition of the blood is closely related to its functions in the body, many of which involve transport.
They include transport of:
- oxygen to, and carbon dioxide from, the respiring cells
- digested food from the small intestine
- nitrogenous waste products from the cells to the excretory organs
- chemical messages (hormones)
- food molecules from storage compounds to the cells that need them
- platelets to damaged areas
- cells and antibodies involved in the immune response.
The blood also contributes to maintenance of a steady body temperature and acts as a buffer, minimising pH changes.
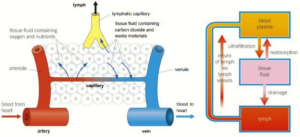
Tissue fluid
The substances dissolved in plasma can pass through the fenestrations in the capillary walls, with the exception of the large plasma proteins.
The plasma proteins, particularly albumin, have an osmotic effect.
They give the blood in the capillaries a relatively high solute potential (and so a relatively low water potential) compared with the surrounding fluid.
As a result, water has a tendency to move into the blood in the capillaries from the surrounding fluid by osmosis.
The tendency of water to move into the blood by osmosis is termed osmotic pressure and it is about –3.3 kPa.
However, as blood flows through the arterioles into the capillaries, it is still under pressure from the surge of blood that occurs every time the heart contracts.
This is hydrostatic pressure.
All the arterial end of the capillary, the hydrostatic pressure forcing fluid out of the capillaries is relatively high at about 4.6kPa.
It is higher than the osmotic pressure attracting water in by osmosis, so fluid is squeezed out of the capillaries.
This fluid fills the spaces between the cells and is called tissue fluid.
Tissue fluid has the same composition as the plasma, without the red blood cells and the plasma proteins.
Diffusion takes place between the blood and the cells through the tissue fluid.
As the blood moves through the capillaries towards the venous system, the balance of forces changes.
The hydrostatic pressure falls to around 2.3 kPa in the vessels as fluid has moved out and the pulse is completely lost.
The osmotic pressure is still -3.3 kPa, so it is now stronger than the hydrostatic pressure, so water moves back into the capillaries by osmosis as it approaches the venules end of the capillaries.
By the time the blood returns to the veins, 90% of the tissue fluid is back in the blood vessels.
Lymph
Some of the tissue fluid does not return to the capillaries.
About 10% of the liquid that leaves the blood vessels drains into a system of blind ended tubes called lymph capillaries, where it is known as lymph.
Lymph is similar in composition to plasma and tissue fluid but has less oxygen and fewer nutrients.
It also contains fatty acids, which have been absorbed into the lymph from the villi of the small intestine.
The lymph capillaries join up to form larger vessels.
The fluid is transported through them by the squeezing of the body muscles.
One-way valves like those in veins prevent the backflow of lymph.
Eventually the lymph returns to the blood, flowing into the right and left subclavian veins (under the clavicle, or collar bone).
Along the lymph vessels are the lymph nodes.
Lymphocytes build up in the lymph node when necessary and produce antibodies, which are then passed into the blood.
Lymph nodes also intercept bacteria and other debris from the lymph, which are ingested by phagocytes found in the nodes.
The lymphatic system plays a major role in the defence mechanisms of the body.
Enlarged lymph nodes are a sign that the body is fighting off an invading pathogen.
This is why doctors often examine the neck, armpits, stomach or groin of their patients, these are the sites of some of the major lymph nodes (which people often refer to as ‘lymph glands’).
It is very important to note that;
Blood is the main transport medium of the human circulatory system, but it is only part of the story.
Tissue fluid is the other important player in the exchange of substances between the blood and the cells.
A third liquid, lymph, is also part of the complex system that makes up the circulation of the body.