Understanding the Hormonal Control of the Male and Female Reproductive System.
Understanding the Hormonal Control of the Male and Female Reproductive System.
Content:
Hormonal control of the male reproductive system.
Hormonal control of the female reproductive cycle
- The Ovarian Cycle
- The Uterine (Menstrual) Cycle
Menopause
Menstrual and Oestrous Cycles
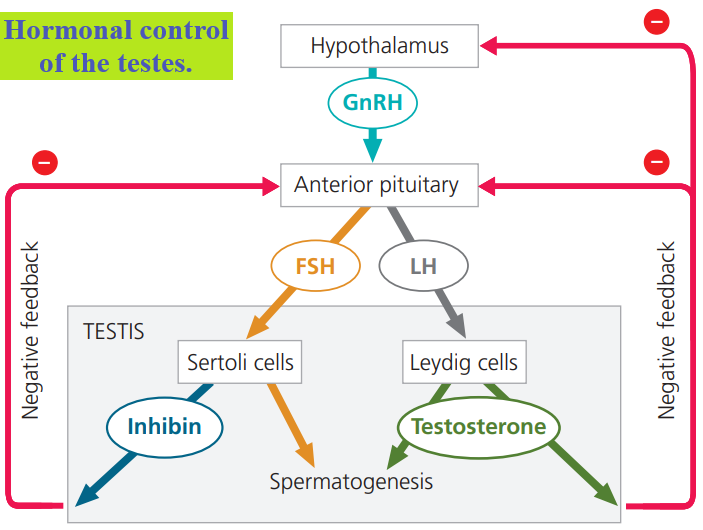
Hormonal control of the male reproductive system.
When mammals reach sexual maturity, the sex hormones and gonadotropins have essential roles in gametogenesis.
In exploring this hormonal control of reproduction, we’ll begin with the relatively simple system found in males.
In directing spermatogenesis, FSH and LH act on two types of cells in the testis.
FSH stimulates Sertoli cells, located within the seminiferous tubules, to nourish developing sperm.
LH causes Leydig cells, scattered in connective tissue between the tubules, to produce testosterone and other androgens, which promote spermatogenesis in the tubules.
Two negative feedback mechanisms control sex hormone production in males.
Testosterone regulates the blood concentration of GnRH, FSH, and LH through inhibitory effects on the hypothalamus and anterior pituitary.
In addition, inhibin, a hormone that in males is produced by Sertoli cells, acts on the anterior pituitary gland to reduce FSH secretion.
Together, these negative feedback circuits maintain the androgen level in the normal range.
Leydig cells have other roles besides producing testosterone.
They secrete small quantities of many other hormones and local regulators, including oxytocin, renin, angiotensin, corticotropin-releasing factor, growth factors, and prostaglandins.
These signals coordinate the activity of reproduction with growth, metabolism, homeostasis, and behaviour.
Hormonal control of the female reproductive cycle
Whereas sperm are produced continuously in human males, there are two closely linked reproductive cycles in human females.
Cyclic patterns of endocrine signalling control both.
Cyclic events in the ovaries define the ovarian cycle:
Once per cycle a follicle matures and an oocyte is released.
Changes in the uterus define the uterine cycle, which in humans and some other primates is a menstrual cycle.
In each menstrual cycle, the endometrium (lining of the uterus) thickens and develops a rich blood supply before being shed through the cervix and vagina if pregnancy does not occur.
By linking the ovarian and uterine cycles, hormone activity synchronizes ovulation with the establishment of a uterine lining that can support embryo implantation and development.
If an oocyte is not fertilized and pregnancy does not occur, the uterine lining is sloughed off, and another pair of ovarian and uterine cycles begin.
The cyclic shedding of the blood-rich endometrium from the uterus, a process that occurs in a flow through the cervix and vagina, is called menstruation.
Menstrual and ovarian cycles average 28 days but can range from about 20 to 40 days.
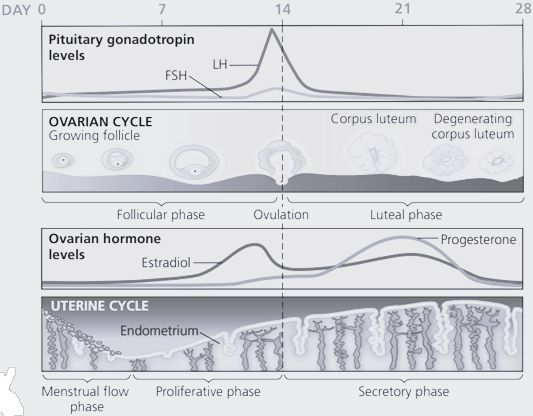
The Ovarian Cycle
In human females, as in males, the hypothalamus has a central role in regulating reproduction.
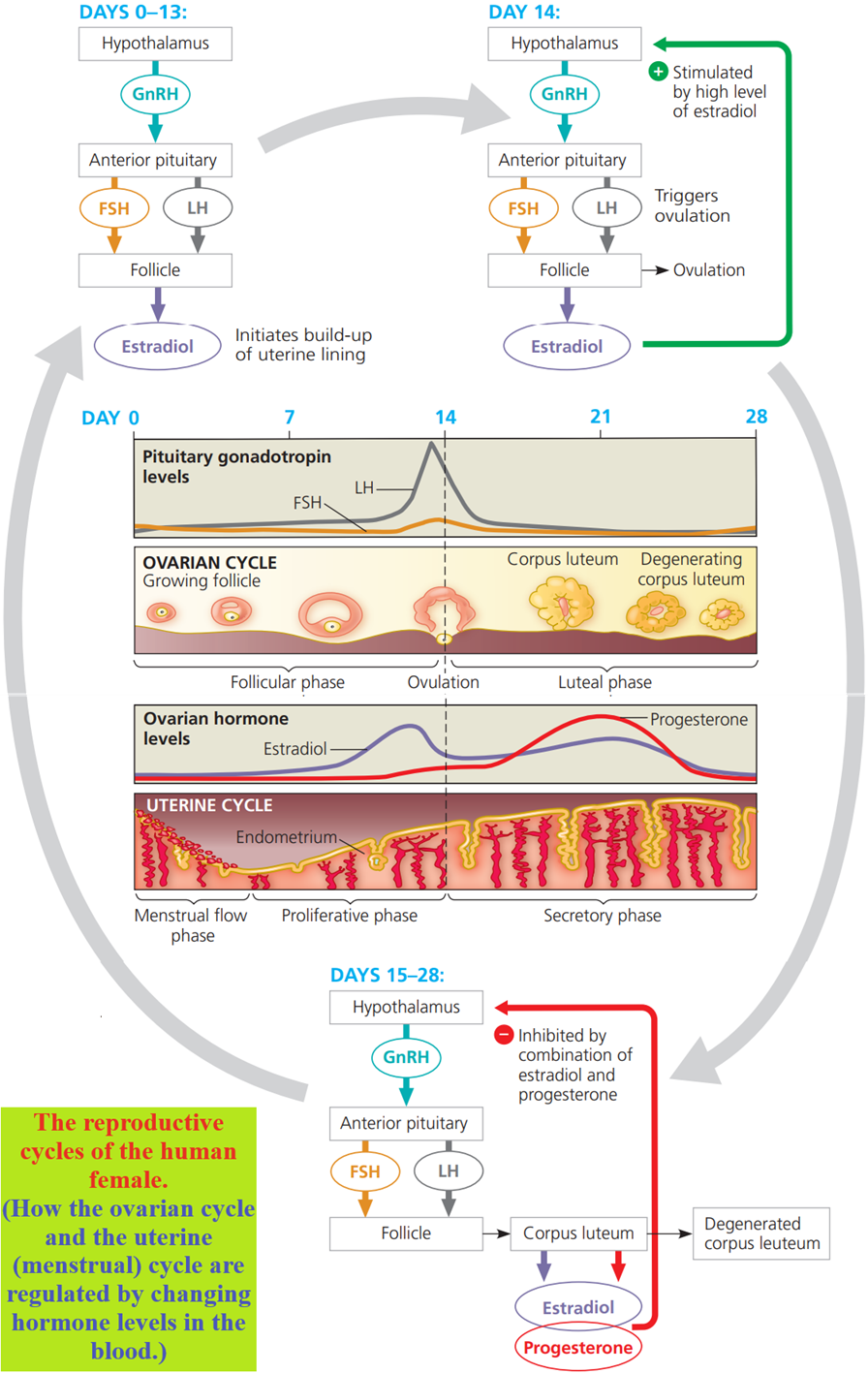
The ovarian cycle begins when the hypothalamus releases GnRH, which stimulates the anterior pituitary to secrete small amounts of FSH and LH.
Follicle-stimulating hormone (as its name implies) stimulates follicle growth, aided by LH, and the cells of the growing follicles start to make oestradiol.
Oestradiol concentration slowly rises during most of the follicular phase (days 0–14), the part of the ovarian cycle during which follicles grow and oocytes mature.
Several follicles begin to grow with each cycle, but usually only one matures; the others disintegrate.
A low concentration of oestradiol inhibits the secretion of pituitary hormones, keeping the concentration of FSH and LH relatively low.
In this portion of the cycle, the regulation of the reproductive hormones closely parallels the regulation in males.
When oestradiol secretion by the follicle begins to rise steeply, the levels of FSH and LH increase markedly.
Why?
Whereas a low level of oestradiol inhibits the secretion of pituitary gonadotropins, a high concentration has the opposite effect.
It stimulates gonadotropin secretion by causing the hypothalamus to increase the output of GnRH.
A high oestradiol concentration also increases the GnRH sensitivity of LH-releasing cells in the pituitary, further increasing the LH level.
The maturing follicle, containing a fluid-filled cavity, enlarges to form a bulge at the surface of the ovary.
The follicular phase ends at ovulation (day 14), about a day after the LH surge. In response to FSH and the peak in LH level, the follicle and adjacent wall of the ovary rupture, releasing the secondary oocyte.
At or near the time of ovulation, women may feel pain in the lower abdomen, on the same side as the ovary that released the oocyte.
The luteal phase (days 15–28) of the ovarian cycle follows ovulation.
LH stimulates the remaining follicular tissue to form the corpus luteum, a glandular structure.
Stimulated by LH, the corpus luteum secretes progesterone and oestradiol, which in combination exert negative feedback on the hypothalamus and pituitary.
This feedback greatly reduces LH and FSH secretion, preventing the maturation of another egg when a pregnancy may be underway.
If pregnancy does not occur, the low gonadotropin concentration at the end of the luteal phase causes the corpus luteum to disintegrate, triggering a sharp decline in oestradiol and progesterone concentrations.
This decline liberates the hypothalamus and pituitary from negative feedback.
The pituitary can then secrete enough FSH to stimulate the growth of new follicles, initiating the next ovarian cycle.
The Uterine (Menstrual) Cycle
Before ovulation, ovarian steroid hormones stimulate the uterus to prepare for support of an embryo.
Oestradiol secreted in increasing amounts by growing follicles signals the endometrium to thicken.
In this way, the follicular phase of the ovarian cycle is coordinated with the uterine cycle’s proliferative phase (days 6–14).
After ovulation, the oestradiol and progesterone secreted by the corpus luteum stimulate maintenance and further development of the uterine lining, including enlargement of arteries and growth of endometrial glands.
These glands secrete a nutrient fluid that can sustain an early embryo even before it implants in the uterine lining.
Thus, the luteal phase of the ovarian cycle is coordinated with the uterine cycle’s secretory phase (days 15–28).
Once the corpus luteum has disintegrated, the rapid drop in ovarian hormone concentration causes arteries in the endometrium to constrict.
Deprived of its circulation, the uterine lining largely disintegrates, releasing blood that is shed along with endometrial tissue and fluid.
The result is menstruation, the menstrual flow phase (days 1–5) of the uterine cycle.
During this phase, which usually lasts a few days, a new set of ovarian follicles begins to grow.
By convention, the first day of flow is designated day 1 of the new uterine (and ovarian) cycle.
About 7% of women of reproductive age suffer from a disorder called endometriosis, in which some cells of the uterine lining migrate to an abdominal location that is abnormal, or ectopic.
Having migrated to a location such as an oviduct, ovary, or large intestine, the ectopic tissue responds to hormones in the bloodstream.
Like the uterine endometrium, the ectopic tissue swells and breaks down during each ovarian cycle, resulting in pelvic pain and bleeding into the abdomen.
Researchers have not yet determined why endometriosis occurs, but hormonal therapy or surgery can be used to lessen discomfort.
Menopause
After about 500 cycles, a woman undergoes menopause, the cessation of ovulation and menstruation.
Menopause usually occurs between the ages of 46 and 54.
During this interval, the ovaries lose their responsiveness to FSH and LH, resulting in a decline in oestradiol production.
Menopause is an unusual phenomenon.
In most other species, females and males can reproduce throughout life.
Is there an evolutionary explanation for menopause?
One intriguing hypothesis proposes that during early human evolution, undergoing menopause after bearing several children allowed a mother to provide better care for her children and grandchildren, thereby increasing the chances for survival of individuals who share much of her genetic makeup.
Menstrual and Oestrous Cycles
In all female mammals, the endometrium thickens before ovulation, but only humans and some other primates have menstrual cycles.
In other mammals, both domesticated and wild, the uterus reabsorbs the endometrium in the absence of a pregnancy, and no extensive fluid flow occurs.
For these animals, the cyclic changes in the uterus occur as part of an oestrous cycle that also controls the sexual receptivity of females:
Whereas human females may engage in sexual activity throughout the menstrual cycle, mammals with oestrous cycles usually copulate only during the period surrounding ovulation.
This period, called oestrus (from the Latin oestrus, frenzy, passion), is the only time the female is receptive to mating.
It is often called “heat,” and the female’s temperature does increase slightly.
- The length, frequency, and nature of oestrous cycles vary.
- Bears and wolves have one oestrous cycle per year; elephants have several.
- Rats have oestrous cycles throughout the year, each lasting just five days.
- The rat’s nemesis, the household cat, ovulates only upon mating.