THE PRINCIPLE OF DISINFECTION
THE PRINCIPLE OF DISINFECTION
Disinfection is the second critical step in reprocessing devices.
To be effective, disinfection must be preceded by thorough cleaning and must be done properly.
Staff members must check the disinfectant’s concentration regularly if it is diluted at the place of use, even if it is diluted with an electronically monitored dilution device.
Failures of the valve or other critical parts of the device can result in an insufficient final concentration, which usually cannot be detected by checking either the appearance or the odor of the disinfectant.
Many manufacturers provide test strips to check for the appropriate concentration.
Numerous outbreaks have occurred when staff members have not followed appropriate protocols.
The goal of disinfection is to kill rather than inhibit the growth of microorganisms.
In contrast to sterilization, but similar to antimicrobial agents, killing curves for disinfectants is not linear and the rate of log killing decreases as the inoculum concentrations decrease.
Commonly Used Disinfectants/ Germicides for Devices.
Formaldehyde:
- Formaldehyde in aqueous solutions or as a gas has been used as a disinfectant and sterilant for many decades.
- Its use in the health care setting, however, has sharply decreased for several reasons.
- The irritating vapours and pungent odor produced by formaldehyde are apparent at very low levels.
- Moreover, allergy to formaldehyde is fairly common.
- In addition, the Occupational Safety and Health Administration and the Health and Safety Executive indicated that formaldehyde vapours may be carcinogenic.
- Consequently, formaldehyde and formaldehyde-releasing agents are used infrequently in healthcare institutions, despite these agents’ broad-spectrum microbicidal activity.
- Formaldehyde has been largely replaced by peracetic acid as an agent for disinfecting haemodialysis equipment and water dialysate tubing systems.
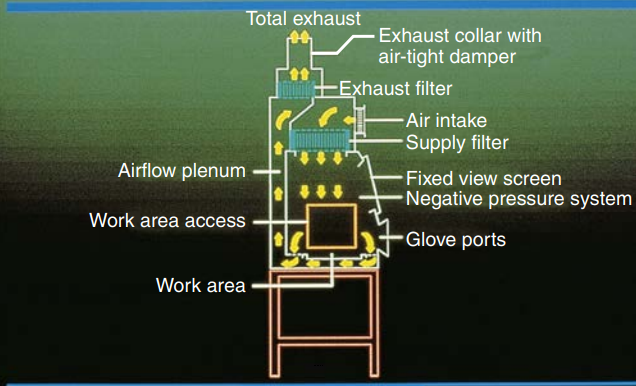
- Paraformaldehyde vaporized by heat is used to decontaminate biological safety cabinets.
Glutaraldehyde:
The biocidal activities of glutaraldehyde solutions are dependent on a variety of variables, such as
- pH,
- temperature,
- concentration at the time of use,
- the presence of inorganic ions,
- and the age of the solution
Aqueous solutions of glutaraldehyde are usually acidic and are not sporicidal in this form.
Therefore, they need to be activated by adding an alkalinizing agent.
These activated solutions, however, rapidly lose their activity because glutaraldehyde molecules polymerize at an alkaline pH.
Therefore, the shelf life of such solutions is limited to 14 days unless the manufacturer recommends otherwise.
The activities of disinfectants increase as the temperature rises.
Among eight disinfectants tested, glutaraldehyde was found to be the chemical most strongly affected by temperature.
Some stable acid glutaraldehyde may be used at temperatures of 35 to 55°C at concentrations below 2%.
Glutaraldehyde retains its activity in the presence of organic.
A standard 2% aqueous solution of glutaraldehyde buffered to pH 7.5 to 8.5 is bactericidal, tuberculocidal, sporicidal, fungicidal, and virucidal.
It rapidly kills both Gram-negative and Gram-positive vegetative bacteria.
Longer exposure times are required to inactivate spores and mycobacteria.
Ortho-phthalaldehyde (OPA):
Compared with glutaraldehyde, OPA has several advantages:
- it does not require activation
- it is compatible with many materials (i.e., similar to glutaraldehyde).
- it is more stable during storage and reuse as well as at a wide pH range of 3 to 9.
- it has low vapor properties.
- its odor is barely perceptible.
- it is more rapidly mycobactericidal than glutaraldehyde in vitro and has good activity against glutaraldehyde-resistant strains at longer exposure times.
However, 0.5% OPA is slowly sporicidal and does not inactivate all spores within 270 minutes of exposure.
In addition, OPA stains proteins, skin, clothing, and instruments.
OPA vapours may irritate the respiratory tract and eyes.
At present, the effects of long-term exposure and safe exposure levels are not well defined.
Therefore, OPA must be handled with appropriate safety precautions (i.e., gloves, fluid-resistant gowns, and eye protection),
It must be stored in containers with tight-fitting lids.
Hydrogen Peroxide:
- Hydrogen peroxide, a strong oxidizer, is used for high-level disinfection and sterilization.
- It produces destructive hydroxyl free radicals that attack membrane lipids, DNA, and other essential cell components.
- Although the catalase produced by anaerobic and some aerobic bacteria may protect cells from hydrogen peroxide, this defense is overwhelmed by the concentrations used for disinfection.
- Generally, a 3% hydrogen peroxide solution is rapidly bactericidal, but it kills organisms with high cellular catalase activity less rapidly.
Peracetic Acid:
- Peracetic acid (or peroxyacetic acid) is a more potent germicidal agent than hydrogen peroxide and was the most active agent in several in vitro studies
- The mechanism of action of peracetic acid has not been fully elucidated, but its mechanism of action is likely to be similar to that of hydrogen peroxide and other oxidizing agents.
- Peracetic acid remains effective in the presence of organic matter.
- At low concentrations, it is considerably less stable than hydrogen peroxide; preparations with appropriate stability have been developed and are commercially available.
- Peracetic acid corrodes steel, galvanized iron, copper, brass, and bronze, and it attacks natural and synthetic rubbers.
- In addition, concentrated solutions can seriously damage the eyes and skin.
Also Read:
-
The Science and Art of Making Vaccines
-
Why does urine comes with varieties of Colour and Odor?
-
The Science of Aging
-
General Principles of Sterilization
Alcohols:
- Alcohols are also excellent products for intermediate-level and low-level disinfection of small, clean surfaces, equipment, and the environment (e.g., rubber stoppers of medication vials, stethoscopes, and medication preparation areas).
- However, alcohol may damage rubber, certain plastic items, and the shellac mountings of lensed instruments after prolonged and repeated use.
- Moreover, alcohols are flammable (one should consider the flash point) and thus must not be used on large surfaces, particularly in closed, poorly ventilated areas.
- Alcohols cannot penetrate protein-rich materials.
- Therefore, a spray or a wipe with alcohol may not disinfect a surface contaminated with blood or other body fluids that have not been cleaned first.
Quaternary Ammonium Compounds:
A wide variety of quaternary ammonium compounds (quats) with antimicrobial activity have been introduced in the past decade.
Some of the compounds used in healthcare settings are;
- benzalkonium chloride,
- alkyldimethylbenzyl ammonium chloride,
- and didecyldimethyl ammonium chloride.
Quats are cationic surface-active detergents, which appear to kill microorganisms by disrupting cell membranes, inactivating enzymes, and denaturing cell protein.
Chlorine and Chlorine-Releasing Compounds:
- Due to its hazardous nature, chlorine gas is rarely used as a disinfectant.
- Among the large number of chlorine compounds commercially available, hypochlorites are the most widely used disinfectants.
- Hypochlorite has been used for more than a century and remains an important disinfectant.
Phenolics:
Phenol derivatives originate when one of the hydrogen atoms on an aromatic ring is replaced by a functional group (e.g., alkyl, benzyl, phenyl, amyl, or chloro).
The three phenolics most commonly used as constituents of disinfectants are
- o-phenylphenol,
- o-benzyl-p-chlorophenol,
- and p-tert-amyl- phenol.
The addition of detergents to the basic formulation results in products that clean, dissolve proteins, and disinfect in one step.
Phenolics at higher concentrations act as gross protoplasmic poisons, penetrating and disrupting the bacteria’s cell wall and precipitating the cell proteins
Other Germicides/disinfectants of Interest:
- Glucoprotamine
- Peroxygen compounds have proven efficacy against bacteria, bacterial spores, fungi, and a broad spectrum of viruses.
- Metals such as copper and silver ions inactivate a wide variety of microorganisms.
Physical Methods of Disinfection
The three physical methods of disinfection are:
- Boiling at 100°C for 15 minutes, which kills vegetative bacteria
- Pasteurizing at 70°C for 30 minutes, which kills food pathogens without damaging the nutritional value.
- Using nonionizing radiation such as ultraviolet (UV) light
- UV rays are long wavelength and low energy. They do not penetrate well, and organisms must have direct surface exposure, such as the working surface of a BSC, for this form of disinfection to work.
Join Enlighten Knowledge WhatsApp platform.
Join Enlighten Knowledge Telegram platform.
Follow our:
FACEBOOK PAGE.