Regulation of Blood Glucose Concentration, Diabetes and its Control.
Regulation of Blood Glucose Concentration, Diabetes and its Control.
Content:
- Increasing and decreasing blood glucose concentration
- Role of insulin blood glucose concentration
- Role of glucagon blood glucose concentration
- Mechanism of controlling insulin secretion
- Islets of Langerhans in the pancreas
- Diabetes Treatment and Control.
- Common symptoms of diabetes
- Types of diabetes (type 1 and type 2 diabetes)
- Treatment of both type 1 and type 2 diabetes
- Medically produced insulin
- Potential use of stem cells in diabetes treatment
- Stem cell therapy
- Advantage of stem cell therapy over other therapies
During respiration, the body uses glucose to produce ATP.
To remain healthy, the concentration of glucose in your blood must be kept constant.
Without control, blood glucose concentration would range from very high levels after a meal to very low levels several hours later.
At these deficient levels, cells would not have enough glucose for respiration.
Blood glucose concentration is kept constant by the action of the two hormones;
- insulin
- and glucagon.
Increasing blood glucose concentration
Glucose is a small soluble molecule that is carried in the blood plasma.
Blood glucose is normally maintained at around 90 mg cm/3 of blood.
Blood glucose concentration can increase as a result of:
Diet:
- When you eat carbohydrate-rich foods such as pasta and rice (which are rich in starch) and sweet foods such as cakes and fruit (which contain high levels of sucrose), the carbohydrates they contain are broken down in the digestive system to release glucose.
- The glucose released is absorbed into the bloodstream, and the blood glucose concentration rises.
Glycogenolysis
- Glycogen stored in the liver and muscle cells is broken down into glucose which is released into the bloodstream increasing blood glucose concentration.
Gluconeogenesis
- The production of glucose from non-carbohydrate sources.
- For example, the liver is able to make glucose from glycerol (from lipids) and amino acids.
- This glucose is released into the bloodstream and causes an increase in blood glucose concentration.
Decreasing blood glucose concentration
Blood glucose concentration can be decreased by:
Respiration
- Some of the glucose in the blood is used by cells to release energy.
- This is required to perform normal body functions.
- However, during exercise, more glucose is needed as the body needs to generate more energy in order for muscle cells to contract.
- The higher the level of physical activity, the higher the demand for glucose and the greater the decrease in blood glucose concentration.
Glycogenesis
- The production of glycogen.
- When blood glucose concentration is too high, excess glucose taken in through the diet is converted into glycogen which is stored in the liver.
Role of insulin in blood glucose concentration
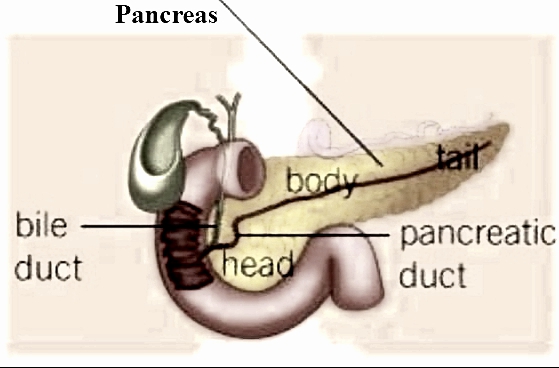
Insulin is produced by the P cells of the islets of Langerhans in the pancreas.
If the blood glucose concentration is too high, the p cells detect this rise in blood glucose concentration and respond by secreting insulin directly into the bloodstream.
Virtually all body cells have insulin receptors on their cell surface membrane (an exception being red blood cells).
When insulin binds to its glycoprotein receptor, it causes a change in the tertiary structure of the glucose transport protein channels.
This causes the channels to open allowing more glucose to enter the cell.
It also activates enzymes within some cells to convert glucose to glycogen and fat.
However, insulin lowers blood glucose concentration by:
- increasing the rate of absorption of glucose by cells, in particular skeletal muscle cells.
- increasing the respiratory rate of cells, increases their need for glucose and causes a higher uptake of glucose from the blood
- increasing the rate of glycogenesis. Insulin stimulates the liver to remove glucose from the blood by turning the glucose into glycogen and storing it in the liver and muscle cells.
- increasing the rate of glucose-to-fat conversion.
- inhibiting the release of glucagon from the cells of the islets of Langerhans.
Insulin is broken down by enzymes in the cells of the liver.
Therefore, to maintain its effect it has to be constantly secreted.
Depending on the food eaten, insulin secretion can begin within minutes of the food entering the body and may continue for several hours after eating.
As blood glucose concentration returns to normal, this is detected by the P cells of the pancreas.
When it falls below a set level, the P cells reduce their secretion of insulin.
This is an example of negative feedback.
Negative feedback ensures that, in any control system, changes are reversed and returned to the set level.
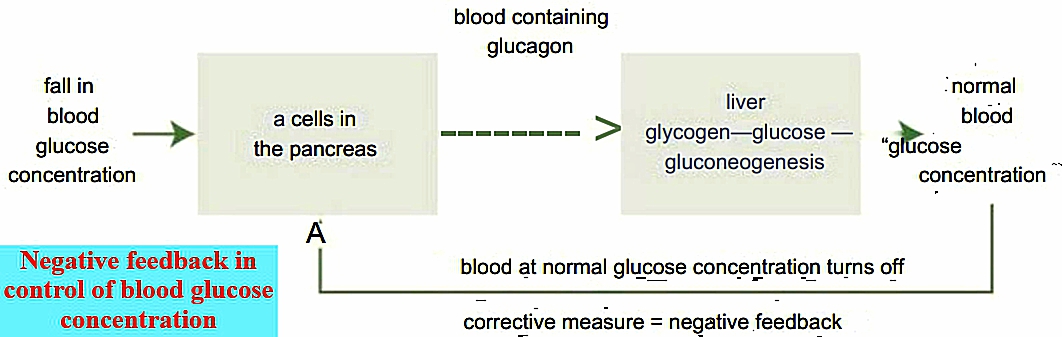
Role of glucagon in blood glucose concentration.
Glucagon is produced by the “a cells” of the islets of Langerhans in the pancreas.
If the blood glucose concentration is too low, the “a cells” detect this fall in blood glucose concentration and respond by secreting glucagon directly into the bloodstream.
Unlike insulin, the only cells in the body which have glucagon receptors are the liver cells and fat cells therefore these are the only cells that can respond to glucagon.
Glucagon raises blood glucose concentration by:
- glycogenolysis; the liver breaks down its glycogen stored into glucose and releases it back into the bloodstream
- reducing the amount of glucose absorbed by the liver cells
- increasing gluconeogenesis. Increasing the conversion of amino acids and glycerol into glucose in the liver.
As blood glucose concentration returns to normal, this is detected by the cells of the pancreas.
When it rises above a set level, the cells reduce their secretion of glucagon.
This is another example of negative feedback.
The feedback causes the corrective measures to be switched off, returning the system to its original (normal) level.
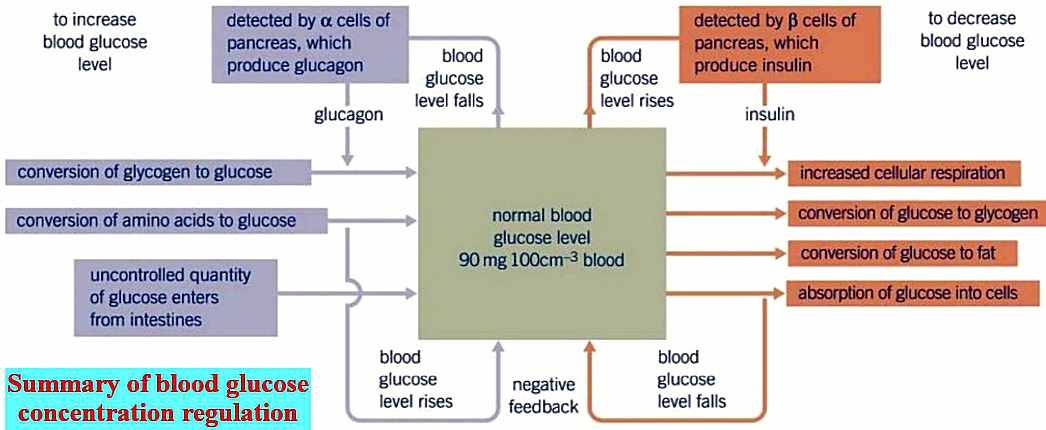
The system of maintaining blood glucose concentration is said to be self-regulating, as it is the level of glucose in the blood that determines the quantity of insulin and glucagon that is released.
Blood glucose concentration is not constant, but fluctuates around a set point as the result of negative feedback.
In times of stress, adrenaline is released by the body.
One of the effects of this hormone is to raise the blood glucose concentration to allow more respiration to occur
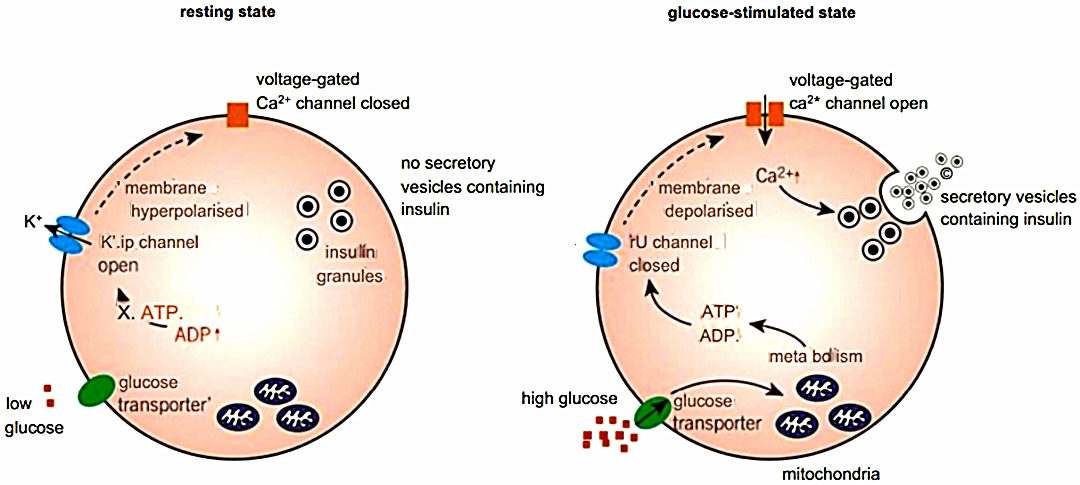
Mechanism of controlling insulin secretion
- When blood glucose concentration rises above the set level this is detected by the P cells in the islets of Langerhans and insulin is released.
The mechanism by which this occurs is as follows:
- At normal blood glucose concentration levels, potassium channels in the plasma membrane of the cells are open and potassium ions diffuse out of the cell. The inside of the cell is at a potential of -70 mV concerning the outside of the cell.
- When blood glucose concentration rises, glucose enters the cell by a glucose transporter.
- The glucose is metabolized inside the mitochondria, resulting in the production of ATP.
- The ATP binds to potassium channels and causes them to close. They are known as ATP-sensitive potassium channels.
- As potassium ions can no longer diffuse out of the cell, the potential difference reduces to around -30 mV and depolarisation occurs.
- Depolarisation causes the voltage-gated calcium channels to open.
- Calcium ions enter the cell and cause secretory vesicles to release the insulin they contain by exocytosis.
Islets of Langerhans in the pancreas
Within the islets of Langerhans are different types of cells.
They are classified according to the hormone they secrete:
- a (alpha) cells – these produce and secrete glucagon
- p (beta) cells – these produce and secrete insulin
Alpha cells are larger and more numerous than beta cells within an islet.
Diabetes Treatment and Control.
- To keep blood glucose concentration constant the body relies on the interaction between glucagon and insulin.
- However, for over 300 million people in the world, this system of regulation does not work properly.
- They suffer from the chronic disease, diabetes mellitus (usually referred to as diabetes).
- This means they are unable to metabolise carbohydrates properly, in particular glucose.
Common symptoms of diabetes
- High blood glucose concentration
- Glucose presents in urine
- Excessive need to urinate [polyuria)
- Excessive thirst (polydipsia)
- Constant hunger
- Weight loss
- Blurred vision
- Tiredness
Types of diabetes
- If you suffer from diabetes your pancreas either does not produce enough insulin, or your body cannot effectively respond to the insulin produced.
- This means that blood glucose concentration remains high.
- Hyperglycaemia, or raised blood sugar, is a common effect of uncontrolled diabetes.
- Over time this can lead to serious damage of many body systems, especially the nerves and blood vessels.
There are two main types of diabetes:
Type 1 diabetes
- Patients with type 1 diabetes are unable to produce insulin.
- The P cells in the islets of Langerhans do not produce insulin.
- The cause of type 1 diabetes is not known and so, al the moment, the disease cannot be prevented or cured.
- It is possible, however, to treat the symptoms.
- Evidence suggests that in many cases the condition arises as a result of an autoimmune response where the body’s own immune system attacks the P cells.
- This condition normally begins in childhood, and people develop symptoms of the disease quickly.
Type 2 diabetes.
- Patients with type 2 diabetes cannot effectively use insulin and control their blood sugar levels.
- This is either because the person’s P cells do not produce enough insulin in the person’s body and cells do not respond properly to insulin.
- This is often because the glycoprotein insulin receptor on the cell membrane does not work properly.
- The cells lose their responsiveness to insulin, and therefore do not take up enough glucose, leaving it in the bloodstream.
- Globally, approximately 90% of people with diabetes have type 2 diabetes.
- This is largely as a result of excess body weight, physical inactivity, and habitual, excessive overeating of (refined) carbohydrates.
- Symptoms are similar to those of type 1 diabetes, but are often less severe and develop slowly.
- As a result, the disease is often only diagnosed after complications have already arisen.
- Risk of type 2 diabetes increases with age.
- Until recently, this type of diabetes was seen only in adults (normally over the age of 40), but it is now also occurring in children.
However, diabetes is not a curable disease, but it can be controlled successfully, allowing sufferers to lead a normal life.
Treatment differs for both types of diabetes.
Type 1 diabetes;
- Type I diabetes is controlled by regular injections of insulin and is therefore said to be insulin-dependent.
- People with the condition have to regularly test their blood glucose concentration, normally by pricking their finger.
- The drop of blood is then analyzed by a machine, which tells the person their blood glucose concentration.
- Based on this concentration, the person can work out the dose of insulin they need to inject.
- The insulin administered increases the amount of glucose absorbed by cells and causes glycogenesis to occur, resulting in a reduction of blood glucose concentration.
- If a person with diabetes injects himself or herself with too much insulin, they may experience hypoglycaemia (very low blood glucose concentrations) that can result in unconsciousness.
- However, too low an insulin dose results in hyperglycaemia, which can also result in unconsciousness and death if left untreated.
- Careful monitoring and dose regulation is therefore required.
- If the person with diabetes injects himself or herself with insulin, there will be a surge of insulin in their blood which will cause their blood glucose level to drop quickly.
Type 2 diabetes
- The first line of control in type 2 diabetes is to regulate the person’s carbohydrate intake through their diet and matching this to their exercise levels.
- This often involves increasing exercise levels.
- Overweight people are also encouraged to lose weight.
- In chronic cases, diet and exercise are not enough to control blood glucose concentration so drugs also have to be used.
- These can include drugs that stimulate insulin production, drugs that slow down the rate at which the body absorbs glucose from the intestine, and ultimately even insulin injections.
Medically produced insulin
- Originally, insulin was obtained from the pancreas of cows and pigs which had been slaughtered for food.
- This process was difficult and expensive.
- The insulin extracted could also cause allergic reactions as it differed slightly from human insulin.
- In 1955, the structure of human insulin was identified and it is now made by genetically modified bacteria.
This has a number of advantages:
- Human insulin is produced in a pure form. This means it is less likely to cause allergic reactions.
- Insulin can be produced in much higher quantities.
- Production costs are much cheaper.
- People’s concerns over using animal products in humans, which may be religious or ethical, are overcome.
Potential use of stem cells in diabetes treatment
- For decades, diabetes researchers have been searching for ways to replace the faulty P cells in the pancreatic islets of diabetic sufferers.
- Each year, over 1000 people with type 1 diabetes receive a pancreas transplant.
- After a year, over 80% of these patients have no symptoms of diabetes and do not have to take insulin.
- However, the demand for transplantable pancreases far outweighs their availability.
- The risk of having a transplant can also be a greater health risk than the diabetes itself.
- Immunosuppressant drugs are required to ensure the body accepts the transplanted pancreas, which can leave a person susceptible to infection.
- Doctors have attempted to cure diabetes by injecting patients with pancreatic P islet cells, but fewer than 8% of cell transplants performed have been successful.
- The immunosuppressant drugs used to prevent rejection of these cells increases the metabolic demand on insulin-producing cells.
- Eventually this exhausts their capacity to produce insulin.
Stem cell therapy
- There is evidence that a relatively small number of islet cells can restore insulin production, the disease is a perfect candidate for stem cell therapy.
- Totipotent stem cells have the potential to grow into any of the body’s cell types.
- Scientists have been researching the best type of stem cells and the signals required to promote their differentiation into P cells, either directly in the patient or in the laboratory before being transplanted.
- It is likely that the stem cells used in diabetes treatment would be taken from embryos.
- To obtain the stem cells, the early embryo has to be destroyed.
- This means destroying a potential human life.
- However, the embryos used as a source for these stem cells would usually be destroyed anyway, they are spare embryos from infertility treatments or from terminated pregnancies.
- Stem cells lines formed from a small number of embryos can be used to treat many patients and each treatment does not require a separate embryo.
- An alternative to using embryonic matter is that of using preserved umbilical stem cells.
Stem cells offer many advantages over current therapies:
- donor availability would not be an issue stem cells could produce an unlimited source of new P cells
- reduced likelihood of rejection problems as embryonic stem cells are generally not rejected by the body (although some evidence contradicts this).
- Stem cells can also be made by somatic cell nuclear transfer (SCNT)
- people no longer have to inject themselves with insulin.
However, because our ability to control growth and differentiation in stem cells is still limited, a major consideration is whether any precursor or stem-like cells transplanted into the body might induce the formation of tumours as a result of unlimited cell growth.
Join Enlighten Knowledge WhatsApp platform.
Join Enlighten Knowledge Telegram platform.