General Principles of Sterilization
General Principles of Sterilization
Sterilization is a process that kills all forms of microbial life, including bacterial endospores.
Many factors limit the success or degree of sterilization such as
- Organic load (organisms and other contaminating materials such as blood or body fluids),
- The type of organisms present,
- The concentration and exposure time to the germicide,
- The physical and chemical nature of the object or surface (hinges, cracks, rough or smooth surfaces),
- Temperature
- PH
- Humidity, and presence of a biofilm.
These processes may be accomplished by a variety of physical or chemical methods.
Sterilization process
The physical methods of sterilization include:
- Incineration
- Moist heat
- Dry heat
- Filtration
- Ionizing (gamma) radiation
- Chemicals (ethylene oxide [EtO] gas, hydrogen peroxide gas plasma, vaporized hydrogen peroxide, and other liquid chemicals)
Incineration
Incineration is a method of treating infectious waste.
A hazardous material is burned to ashes at temperatures of 870°C to 980°C.
Incineration is the safest method to ensure that no infective materials remain in samples or containers when disposed of.
Prions (infective proteins) are not eliminated using conventional methods.
Therefore, incineration is recommended.
Toxic air emissions and the presence of heavy metals in ash have limited the use of incineration.
Also Read:
The Science and Art of Making Vaccines
understanding VIRUS
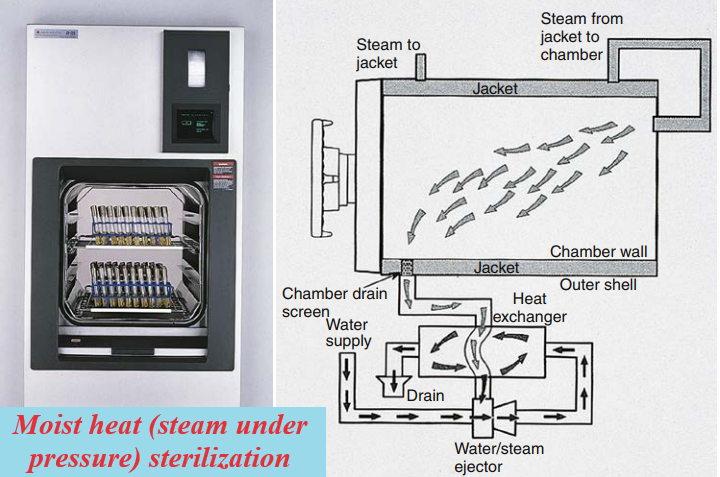
Moist heat (steam under pressure)
It is used to sterilize biohazardous trash and heat-stable objects; an autoclave is used for this purpose.
An autoclave is essentially a large pressure cooker.
Moist heat in the form of saturated steam under one atmosphere (15 pounds per square inch [psi]) of pressure causes the irreversible denaturation of enzymes and structural proteins.
There are four methods for moist heat sterilization:
- autoclave at 134°C for 18 minutes in a pre-vacuum sterilizer
- autoclave at 132°C for 1 hour in a gravity displacement sterilizer;
- immerse in 1 N sodium hydroxide for 1 hour, remove and rinse with water, then autoclave at 121°C in a gravity displacement or 134°C in a pre-vacuum sterilizer for 1 hour;
- immerse in 1 N sodium hydroxide for 1 hour and heat in a gravity displacement at 121°C for 30 minutes, then clean and subject to routine equipment sterilization.
The most commonly used steam sterilizer in the microbiology laboratory is the gravity displacement autoclave.
Steam enters at the top of the sterilizing chamber; because steam is lighter than air, it displaces the air in the chamber and forces it out the bottom through the drain vent.
The two common sterilization temperatures are 121°C and 132°C.
Biologic waste that includes broth or solid media is usually autoclaved for 30 minutes at 121°C in a displacement sterilizer or 4 minutes at 132°C in a pre-vacuum sterilizer.
Infectious medical waste containing body fluids or blood, on the other hand, is often sterilized at 132°C for 30 to 60 minutes to allow penetration of the steam throughout the waste and the displacement of air trapped inside the autoclave bag.
Prions require a much more extensive sterilization process.
Several options are recommended for the removal of prions from surgical instruments or other laboratory materials contaminated with high-risk tissue such as the brain, spinal cord, and eye tissue.
Moist heat is the fastest and simplest physical method of sterilization.
Dry heat and filtration.
It requires longer exposure times (2 to 3 hours) and higher temperatures than moist heat (160° to 180°C).
Dry heat ovens are used to sterilize items such as glassware, oil, petrolatum, or powders.
Filtration is the method of choice for antibiotic solutions, toxic chemicals, radioisotopes, vaccines, and carbohydrates, which are all heat-sensitive.
Sometimes, the filtration of liquids is accomplished by pulling the solution through a cellulose acetate or cellulose nitrate membrane with a vacuum.
Filtration of air is accomplished using high-efficiency particulate air (HEPA) filters designed to remove organisms larger than 0.3μm from isolation rooms, operating rooms, and biological safety cabinets (BSCs).
Although considered a method of sterilization, filtration simply removes micro-organisms and particles larger than the pore size; smaller particles will not be removed using this method.
Ionizing (gamma) radiation and chemical sterilant.
The ionizing radiation used in microwaves and radiograph machines is composed of short-wavelength and high-energy gamma rays.
Ionizing radiation is used for sterilizing disposables such as plastic syringes, catheters, or gloves before use.
The most common chemical sterilant is EtO, which is used in gaseous form for sterilizing heat-sensitive objects.
The main disadvantages of EtO use are the lengthy cycle times and the potential health hazards it produces.
Vapor-phase hydrogen peroxide (an oxidizing agent) has been used to sterilize HEPA filters in BSCs, metals, and nonmetal devices such as medical instruments (e.g., scissors).
There are no toxic byproducts produced using vapor-phase hydrogen peroxide.
Hydrogen peroxide gas plasma is another method that uses hydrogen peroxide and generates plasma by exciting the gas in an enclosed chamber under a deep vacuum with the use of radiofrequency or microwave energy.
Join Enlighten Knowledge WhatsApp platform.
Join Enlighten Knowledge Telegram platform.
Follow our:
FACEBOOK PAGE.